 Ashley Maister, BS, PharmD, BCPP
Ashley Maister, BS, PharmD, BCPP
Clinical Pharmacy Practitioner, Psychiatry
Corporal Michael J. Crescenz Veterans Affairs Medical Center
Philadelphia, Pennsylvania
Dr. Maister received her Doctor of Pharmacy degree from Thomas Jefferson University in 2018 followed by her PGY-1 pharmacy residency at Penn Presbyterian Medical Center and PGY-2 psychiatric pharmacy residency at Ernest Mario School of Pharmacy at Rutgers University. Dr. Maister is Board Certified in Psychiatric Pharmacy, and currently works in an outpatient behavioral health clinic. She serves as a preceptor for both students and residents and was awarded her facility’s Preceptor of the Year award in 2022. Her contributions to the profession also extend to involvement with local and national pharmacy organizations.
The Layered Learning Model
The layered learning model is a way to differentiate instruction to accommodate for different skills and abilities. At its core, it is an effective way to increase trainees’ learning on experiential rotations by allowing them to learn side by side. As a student pharmacist, I enjoyed being on a rotation with a pharmacy resident because I felt like I related to them more as a peer, and thus, was comfortable asking them questions or sharing my ideas with them before meeting with our preceptor. As a pharmacy resident, I enjoyed being on a rotation with a student pharmacist because I was able to model clinical thinking skills and assist my preceptor with instructing psychiatric disease states and medication information. These experiences helped me preferentially plan my rotation availability to allow for “layering” of trainees. Trainees have consistently shared with me that they have learned and experienced more on their rotation because of incorporating the layered learning model.
Benefits and Challenges of Layered Learning
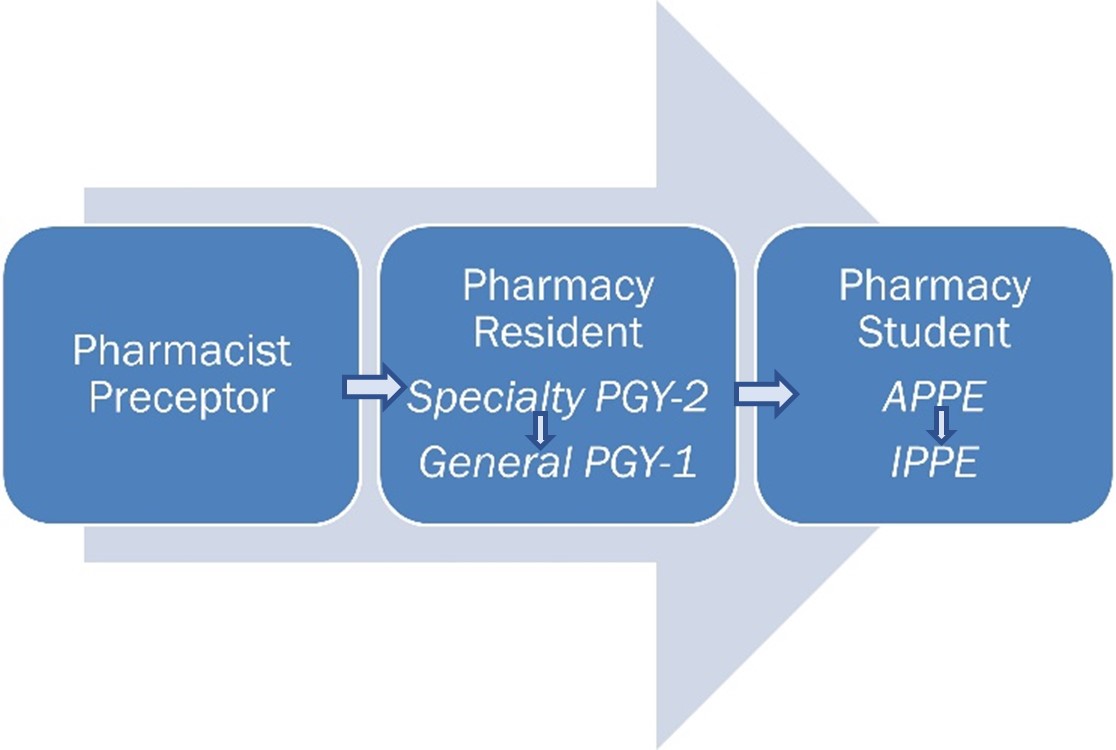
There are several benefits to incorporating the layered learning model into your rotation for all members of the ‘continuum’. The pharmacist preceptor will help to organize and oversee each trainee’s experience; however, as the image suggests, layers even exist within each role. This allows for increased opportunities for direct patient care by all continuum members. Subsequently, the pharmacist preceptor will have more time to work on other responsibilities such as projects, committee tasks, and involvement in professional organizations while still ensuring an enriched learning environment for those on rotation. The pharmacy resident will be able to practice precepting skills by assisting the pharmacist preceptor with direct instruction of student pharmacists, as well as modeling professional behaviors. By helping to precept student pharmacists, the resident is then able to increase independence and autonomy while providing direct patient care. The student pharmacists’ learning experiences will be maximized overall, given their opportunity for one-on-one personalized learning and seeing firsthand how clinical pharmacy can be pursued as a career path.
While I truly enjoy incorporating the layered learning model into my rotations, there are challenges to work through. In order to ‘employ’ a pharmacy resident into a preceptor role, it is important to consider their clinical competency and dependability. For example, I typically find PGY-1 pharmacy residents are more confident in themselves clinically during winter and spring rotations. Thus, rotations during this time may optimize their ability to practice precepting skills with APPE students. If the rotation is earlier in the residency year, the pharmacist preceptor may need to help facilitate the resident’s clinical learning more closely. In addition, inconsistencies between the teaching styles of both the pharmacist preceptor and pharmacy resident may exist, which can create a more difficult learning environment for a student pharmacist. It is also important to consider each person’s individual schedule, such as days off and rotation start and end dates. Mismatches in the schedules may leave gaps in teaching if not addressed. Finally, the size and location of your institution may also limit the overall number of trainees that complete rotations with you, making this method of learning more difficult.
Incorporating Layered Learning into Your Trainee Rotations
Despite the challenges and considerations, you have decided to incorporate layered learning into your rotation. The image below has been simplified to highlight key responsibilities for each ‘layer’ on my outpatient behavioral health clinic rotation:
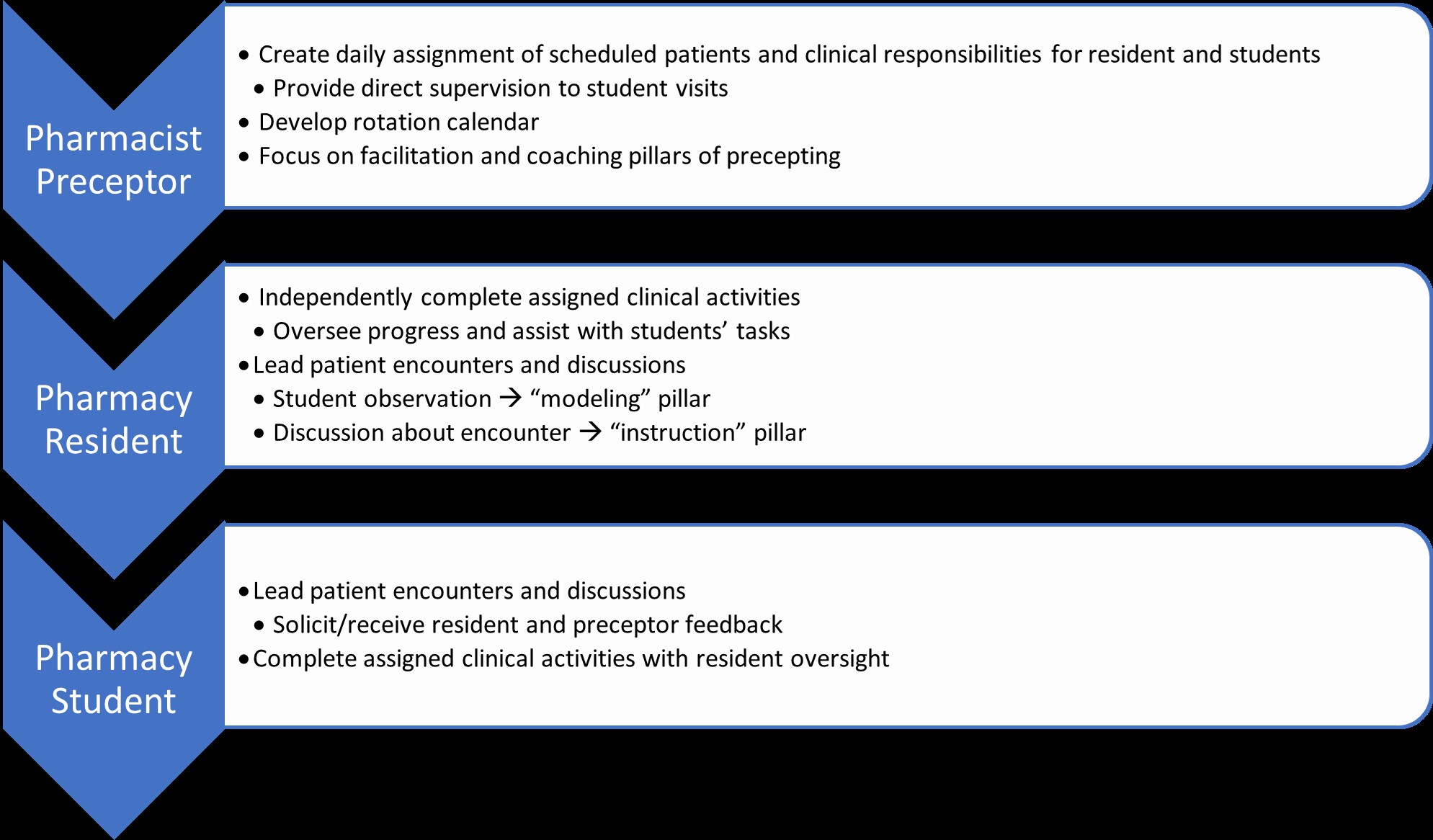
Prior to starting the rotation, plan to discuss your expectations for layered learning with your resident to determine the level at which they feel interested, comfortable, and prepared to participate. Additionally, building in time for the student and resident to provide feedback for each other is another valuable aspect to the layered learning model.
- Pinelli NR, Eckel SF, Vu MB, et al. The layered learning practice model: lessons learned from implementation. Am J Health Syst Pharm. 2016;73(24): 2077-82.
- Loy BM, Yang S, Moss JM, et al. Application of the layered learning practice model in an academic medical center. Hosp Pharm. 2017;52(4): 266-72.
