![]() Download this fact sheet as a PDF to save and print.
Download this fact sheet as a PDF to save and print.
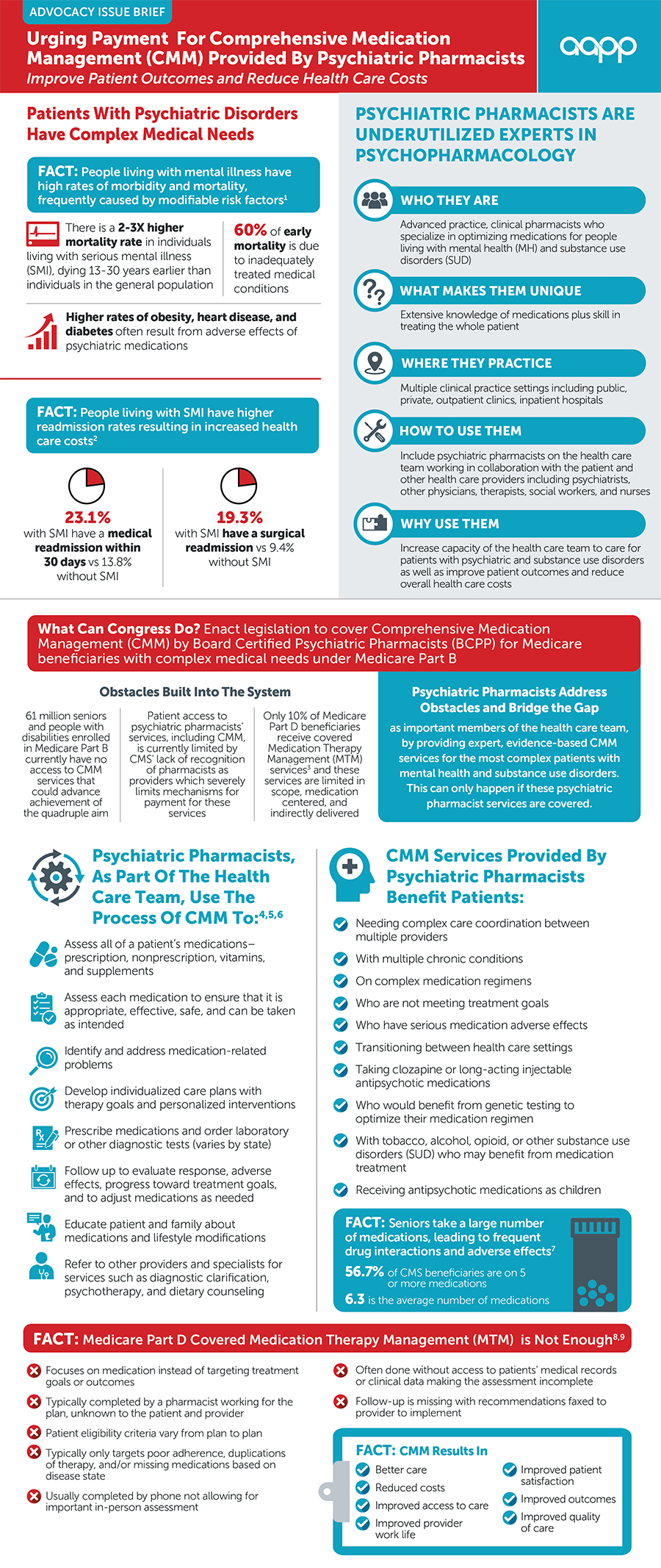
References are located at the bottom of this page.
References
- Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature Mortality Among Adults With Schizophrenia in the United States. Jama Psychiatry. 2015;72(12):1172-81. DOI: 10.1001/jamapsychiatry.2015.1737. PubMed PMID: 26509694.
- De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77. DOI: 10.1002/j.2051-5545.2011.tb00014.x. PubMed PMID: 21379357.
- Germack HD, Noor-E-Alam M, Wang X, Hanrahan N. Association of Comorbid Serious Mental Illness Diagnosis With 30-Day Medical and Surgical Readmissions. Jama Psychiatry. 2019;76(1):96-98. DOI: 10.1001/jamapsychiatry.2018.3091. PubMed PMID: 30476934.
- Stuart B, Hendrick FB, Shen X, Dai M, Tom SE, Dougherty JS, et al. Eligibility For And Enrollment In Medicare Part D Medication Therapy Management Programs Varies By Plan Sponsor. Health Aff (millwood). 2016;35(9):1572-80. DOI: 10.1377/hlthaff.2016.0258. PubMed PMID: 27605635.
- National Board of Medication Therapy Management, Thomas, D. & Tran, J. (2020, September 1). Medication Therapy Management. National Board of Medication Therapy Management https://www.nbmtm.org/mtm-reference/comprehensive-medication-management-versus-comprehensive-medication-review/
- PCPCC Medication Management Task Force. (2012). Integrating Comprehensive Medication Management to optimize patient outcomes resource guide. https://www.pcpcc.orghttps://s.aapp.plus/public/archive-files/media/medmanagement.pdf
- The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings. CMM in Primary Care Research Team. July 2018. Available at http://www.accp.com/cmm_care_process
- Ellenbogen MI, Wang P, Overton HN, Fahim C, Park A, Bruhn WE, et al. Frequency and Predictors of Polypharmacy in US Medicare Patients: A Cross-Sectional Analysis at the Patient and Physician Levels. Drugs Aging. 2020;37(1):57-65. DOI: 10.1007/s40266-019-00726-0. PubMed PMID: 31782129.
- Viswanathan M, Kahwati LC, Golin CE, et al. Medication Therapy Management Interventions in Outpatient Settings [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014 Nov. (Comparative Effectiveness Reviews, No. 138.) Discussion. Available from: https://www.ncbi.nlm.nih.gov/books/NBK294491/
- Ferreri SP, Hughes TD, Snyder ME. Medication Therapy Management: Current Challenges. IPRP. 2020;Volume 9:71- 81. DOI: 10.2147/IPRP.S179628. PubMed PMID: 32309200; PubMed Central PMCID: PMC7136570.
