![]() Download this fact sheet as a PDF to save and print.
Download this fact sheet as a PDF to save and print.
References are located at the bottom of this page.
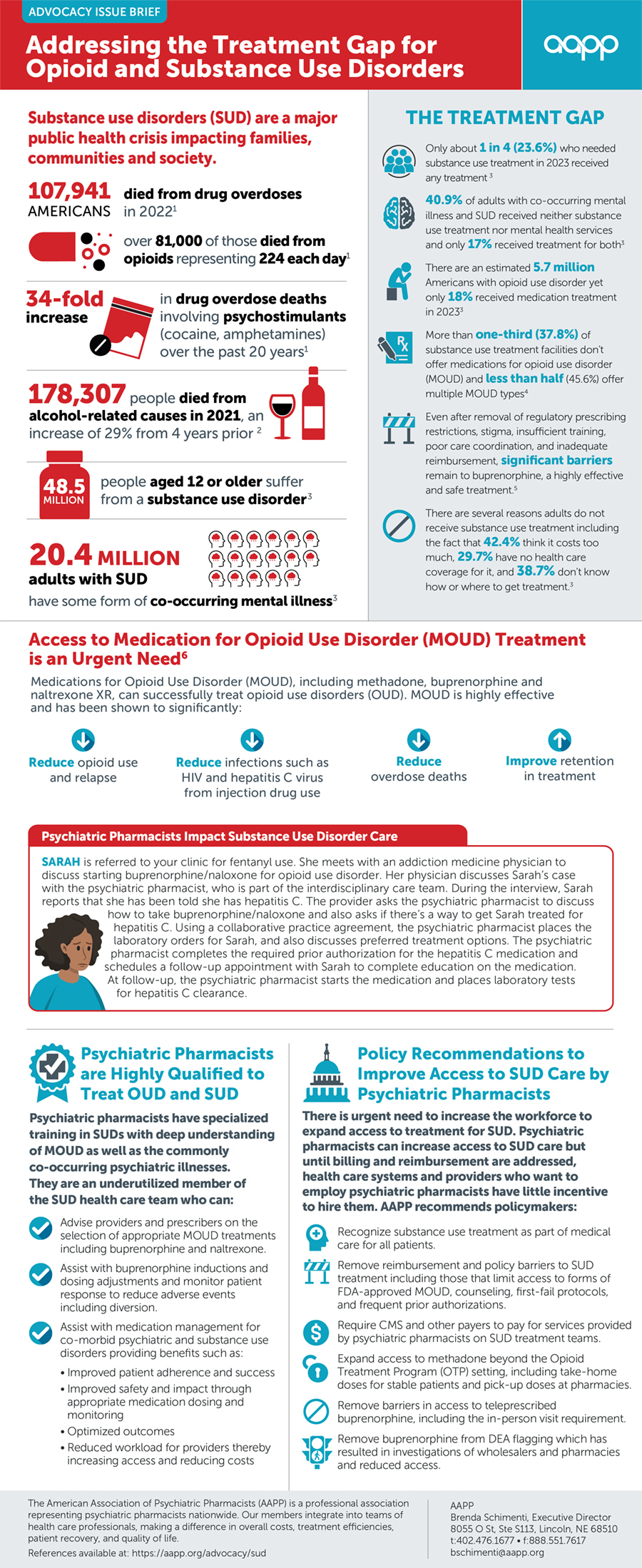
Substance use disorders (SUD) are a major public health crisis impacting families, communities and society. Access to Medication-Assisted Treatment is an Urgent Need 20.3 million people needed treatment for SUD in 2018 but only 3.7 million received treatment 51.4% of individuals with co-occurring mental illness and SUD received neither substance use treatment nor mental health services and only 7.8% received treatment for both Only 7.9% of adults who had alcohol use disorder in the past year received treatment There are fewer than 1,700 programs providing methadone to approximately 380,000 Americans <7% of physicians have DEA waivers to provide MAT Only 13% of clinicians prescribe at or near the authorized waiver patient limit >50% of U.S. counties lack even one buprenorphine provider THE TREATMENT GAP 67,367 AMERICANS died from drug overdoses in 2018 nearly 47,000 of those die from opioids representing 185 each day people aged 12 or older su er from a substance use disorder people die from alcohol-related causes annually, making alcohol the third leading preventable cause of death in the U.S. 20.3 MILLION adults with SUD have some form of co-occurring mental illness 9.2 MILLION Medication-Assisted Treatment (MAT) with methadone, buprenorphine and naltrexone XR can successfully treat opioid use disorders (OUD). MAT is highly e ective and has been shown to: Reduce overdose deaths Improve retention in treatment Reduce opioid use and relapse Reduce infections such as HIV and hepatitis C virus from injection drug use 95,000 To use buprenorphine in SUD treatment, U.S. physicians and other approved professionals must have DEA waivers, also known as DATA or X-waivers. These requirements lead to significant gaps in access to treatment increasing harm and deaths. Psychiatric pharmacists have specialized training in SUDs with deep understanding of MAT as well as the commonly co-occurring psychiatric illnesses. They are an underutilized member of the SUD health care team who can: Policy Recommendations to Improve Access to SUD Care by Psychiatric Pharmacists There is urgent need to increase the workforce to expand access to treatment for SUDs. Psychiatric pharmacists can increase access to SUD care but until billing and reimbursement are addressed, health care systems and providers who want to employ psychiatric pharmacists have little incentive to hire them. CPNP recommends policymakers: Advise providers and waivered prescribers on the selection of appropriate MAT treatments including buprenorphine and naltrexone. Assist with buprenorphine inductions and dosing adjustments and monitor patient response to reduce adverse events including diversion. Assist with medication management for co-morbid psychiatric and substance use disorders providing benefits such as: • Improved patient adherence and success • Improved safety and impact through appropriate medication dosing and monitoring • Optimized outcomes • Reduced workload for providers thereby increasing access and reducing costs Recognize addiction treatment as part of medical care for all patients. Remove reimbursement and policy barriers to SUDs treatment including those that limit access to forms of FDA-approved MAT, counseling, first-fail protocols, and frequent prior authorizations. Require CMS and other payers to pay for services provided by psychiatric pharmacists. Remove the X-waiver requirement and allow buprenorphine to be utilized like other Schedule III drugs. In the absence of the elimination of the X-waiver, add psychiatric pharmacists to the list of providers allowed to obtain waivers to prescribe opioid addiction treatments like buprenorphine.
References
- Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. NCHS Data Brief, no 491. Hyattsville, MD: National Center for Health Statistics. 2024. DOI: https://dx.doi.org/10.15620/cdc:135849
- . Deaths from Excessive Alcohol Use — United States, 2016–2021. Mmwr Morb. Mortal. Wkly. Rep. 2024;73(8):154- 161. DOI: 10.15585/mmwr.mm7308a1. PubMed PMID: 38421934; PubMed Central PMCID: PMC10907037.
- Substance Abuse and Mental Health Services Administration. (2024). Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health (HHS Publication No. PEP24-07-021, NSDUH Series H-59). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2023-nsduh-annual-national-report
- . Treatment Approaches for Opioid Use Disorder Offered in US Substance Use Treatment Facilities. JAMA. 2024;332(6):502. DOI: 10.1001/jama.2024.11913. PubMed PMID: 38990551.
- . Barriers and Facilitators to the Use of Medications for Opioid Use Disorder: a Rapid Review. J Gen Intern Med. 2020;35(S3):954- 963. DOI: 10.1007/s11606-020-06257-4. PubMed PMID: 33145687; PubMed Central PMCID: PMC7728943.
- Substance Abuse and Mental Health Services Administration. Medications for Opioid Use Disorder. Treatment Improvement Protocol (TIP) Series 63 Publication No. PEP21-02-01-002. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2021.
